Diverticulosis and Diverticulitis
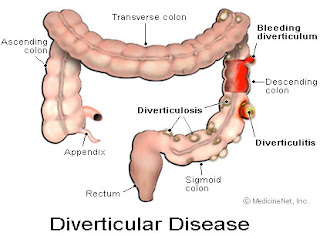
Diverticular disease affects the lining of the bowel. It is caused by small pouches (called diverticula) that can form anywhere in your digestive tract. They occur when the inner layer of the digestive tract bulges through weak spots in the outer layer.
Although these pouches can occur anyplace from the mouth to the anus, most occur in the large intestine (colon), especially the left (lower) part of the colon just above the rectum. These marble-sized pouches usually occur where blood vessels run through the intestinal wall. People who have these pouches are said to have diverticulosis. When this condition does not cause any symptoms, most people are unaware that they have it.
 Sometimes when one or more of these pouches becomes inflamed or infected, a condition called diverticulitis is developed. Some people with diverticulosis become aware of the condition only when diverticulitis occurs. Diverticulosis is a very common condition in the United States. Diverticulosis is more common in developed or industrialized countries. In places such as the United States, England, and Australia, where the typical diet is low in fiber and high in highly processed carbohydrates, diverticulosis is common.
Sometimes when one or more of these pouches becomes inflamed or infected, a condition called diverticulitis is developed. Some people with diverticulosis become aware of the condition only when diverticulitis occurs. Diverticulosis is a very common condition in the United States. Diverticulosis is more common in developed or industrialized countries. In places such as the United States, England, and Australia, where the typical diet is low in fiber and high in highly processed carbohydrates, diverticulosis is common.
Diverticulosis first appeared in the United States in about 1900. This was the same time that processed foods were first introduced into the US diet.
Diverticulosis is much less common in countries of Asia and Africa, where the typical diet is high in fiber.
Most people recover from diverticulitis without problems if they receive appropriate treatment. Diverticulosis and diverticulitis can be prevented by changes in lifestyle and habits.
Causes
Diverticula are thought to be caused by increased pressure within the lumen ( inner aspect ) of the colon. Increased intra-colonic pressure secondary to constipation may lead to weaknesses in the colon walls giving way to diverticula. Fiber causes stools to retain more water and become easier to pass (either soluble or insoluble fiber will do this). A diet without sufficient fiber makes the stools small, requiring the bowel to squeeze harder to remove the smaller stool, thus increasing pressure.
Risk factors
1. Low fiber or high fat diets
2. Elderly
3. Constipation
4. Connective tissue disorders ( cause weakness in the colon wall such as Marfan syndrome).
Symptoms
Diverticulosis has almost no symptoms. The most common is bleeding (variable amounts), bloating, abdominal pain/cramping after meals or otherwise often in the left lower abdomen, and changes in bowel movements (diarrhea or constipation).
Sometimes, symptoms include nonspecific chronic discomfort in the lower left abdomen, with occasional acute episodes of sharper pain. The discomfort is sometimes described as a general feeling of pressure in the region, or pulling sensation. As a general rule, bleeding from the rectum should be followed up with a physician, especially if over age 40 because of the possibility of colon cancer. When blleding is large, symptoms of anemia may present: fatigue, light-headedness, or shortness of breath.
Diagnosis
Your doctor may check your abdomen for tenderness and ask you about your bowel habits, diet and medications. Then, a digital rectal examination might be performed to check for rectal problems. Also, a chemistry blood set might be ordered to check for anemia. Other tests to check for diverticular disease might include:
1. Barium Enema. For this test, you are given an enema (injection of fluid into the rectum) with a liquid that makes your colon show up on an x-ray.
2. Colonoscopy. Before you have this test, you are given a medicine to make you relaxed and sleepy. A thin, flexible tube connected to a video camera is put into your rectum, which allows your doctor to see your whole colon. A colonoscopy may be uncomfortable, but it is usually not painful.
3. CT Scan. Will allow to see the diverticula in your digestive tract that are inflamed or infected.
Complications
Infection of a diverticulum can result in diverticulitis. This occurs in 10-25% of persons with diverticulosis .
Other complications include bleeding or perforations, intestinal obstruction, peritonitis, abscess formation, retroperitoneal fibrosis, sepsis, and fistula formation.
Infection of a diverticulum often occurs as a result of stool collecting in a diverticulum.
Treatment
Dietary
A. Adopt a high-fiber diet. This means lots of fruits and vegetables, whole grains, and cereals. Avoid eating processed foods such as deep fried foods, white bread, crakers, white sugar, artificial sweeteners, etc.
B. Add a fiber supplement to your diet. Take psyllium seed bulking agents. Follow the directions on the package and be sure to take with plenty of water.
C. For constipation, increase your psyllium and water Intake, and if this doesn’t work add bran to your diet. You can take it in tablet form, available in health food stores.
D. Drink plenty of fluids every day: from six to eight glasses of water or other fluid.

Other symptoms such as bloating or abdominal pain may benefit from anti- spasmodic drugs such as chlordiazepoxide (Librax), dicyclomine (Bentyl), Donnatal, and hyoscyamine (Levsin). Some doctors also recommend avoidance of nuts, corn, and seeds to prevent complications of diverticulosis. Whether these diet restrictions are beneficial is uncertain and is not supported by research.
When diverticulitis occurs, antibiotics are usually needed. Oral antibiotics are sufficient when symptoms are mild. Some examples of commonly prescribed antibiotics include ciprofloxacin (Cipro), metronidazole (Flagyl), etc . Liquid or low fiber foods are advised during acute diverticulitis attacks.
Surgical treatment for diverticulitis
Diverticulitis that does not respond to medical treatment requires surgical intervention. Surgery’s goal is to drain any collections of pus and resection of that segment of the colon containing the diverticuli, usually the sigmoid colon. Therefore, surgical removal of the bleeding diverticula is necessary for those with persistent bleeding. Sometimes, diverticula can invade the adjacent bladder, causing severe recurrent urine infection and passage of gas during urination. This situation also requires surgery. Sometimes, surgery may be suggested for patients with frequent, recurrent attacks of diverticulitis leading to multiple courses of antibiotics, hospitalizations, and days lost from work.
Alternative Medicine
On top of the dietary approaches mentioned above, add fish and flax seed oil which will lubricate the colon, add probiotics for digestion, and magnesium for intestine motility.
Acupuncture and Acupressure can certaily help with constipation, bloating and abdominal pain. Points recommended include CV6, LI4, ST36.
Homeopathic preparations are, as usual varied and depending on symptoms. Please go to http://www.hpathy.com/diseases/constipation1-symptoms-treatment-cure.asp

Leave a Reply