Plantar Fasciitis
Are your first steps out of bed in the morning causing you severe pain in your heel? Or does your heel hurt after jogging or playing tennis?
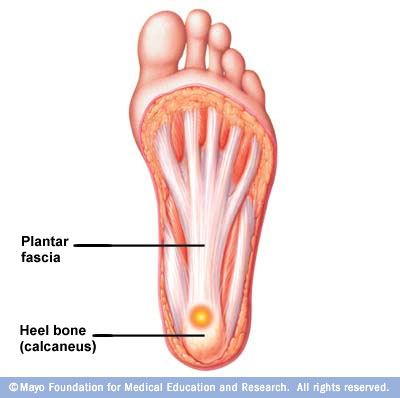
Most commonly, heel pain is caused by inflammation of the plantar fascia which is a tendon, that starts at your heel and goes along the bottom of your foot. It attaches to each one of the bones that form the ball of your foot. The plantar fascia works like a rubber band between the heel and the ball of your foot to form the arch of your foot. If the band is short, you’ll have a high arch, and if it’s long, you’ll have a low arch, what some people call flatfeet. A pad of fat in your heel covers the plantar fascia to help absorb the shock of walking. Damage to the plantar fascia can be a cause of heel pain. The condition is called plantar fasciitis
Plantar fasciitis causes stabbing or burning pain that’s usually worse in the morning because the fascia tightens (contracts) overnight. Once your foot limbers up, the pain of plantar fasciitis normally decreases, but it may return after long periods of standing or after getting up from a seated position.
Risk Factors and Causes
When we age, the plantar fascia becomes less like a rubber band and more like a rope ( stiffens up ) and is unable to stretch very well. The fat pad on the heel becomes thinner and can’t absorb as much of the shock caused by walking. What happens next is that plantar fascia may swell, tear or bruise. You may notice a bruise or swelling on your heel.
- Physical activity overload. Plantar fasciitis is common in long-distance runners. Jogging, walking or stair climbing also can place too much stress on your heel bone and the soft tissue attached to it, especially as part of an aggressive new training regimen.
- Arthritis. Some types of arthritis can cause inflammation in the tendons in the bottom of your foot, which may lead to plantar fasciitis.
- Diabetes. Plantar fasciitis occurs more often in people with diabetes.
- Faulty foot mechanics. Being flat-footed, having a high arch or even having an abnormal pattern of walking can adversely affect the way weight is distributed when you’re on your feet, putting added stress on the plantar fascia.
- Use of improper shoes. Shoes that are thin-soled ( as flip-flops do ) , loose, or lack arch support or the ability to absorb shock don’t protect your feet. If you regularly wear shoes with high heels, your Achilles tendon — which is attached to your heel — can contract and shorten, causing strain 6. Overweight and obesity
- Spending most of the day on your feet
Signs and symptoms
Plantar fasciitis usually develops gradually, but it can come on suddenly and be severe. And although it can affect both feet, it more often occurs in only one foot at a time. Signs and symptoms include:
- A sharp or knife-like pain in the inside part of the bottom of your heel or bottom of foot.
- Heel pain that tends to be worse with the first few steps after awakening, when climbing stairs or when standing on tiptoes.
- Heel pain after long periods of standing or after getting up from a seated position
- Heel pain after, but not usually during, exercise
- Swelling in your heel
Treatment
It typically takes six to eighteen months to find a favorable resolution to plantar fasciitis, but it has a generally good long-term prognosis.
1. Stretching Exercises
- Stretching exercises ( need to be done at home constantly ). The mainstays of treatment are stretching the Achilles tendon and plantar fascia, resting, keeping off the foot as much as possible, discontinuing aggravating activity. Common sense recommendations include wearing supportive and stable shoes. Patients should avoid open-back shoes, sandals, “flip-flops”, and any shoes without a raised heel. Two of the preferred exercises that are usually recommended are:
- A. Towel stretch: Sit on a hard surface with your injured leg stretched out in front of you. Loop a towel around the ball of your foot and pull the towel toward your body keeping your knee straight. Hold this position for 15 to 30 seconds then relax. Repeat 3 times.
- When the towel stretch becomes to easy, you may begin doing the standing calf stretch.
- B. Frozen can roll: Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if done first thing in the morning.
- C. Towel pickup: With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel.
2. Physical Therapy Modalities:
- A physical therapist can instruct you in exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilize your ankle and heel. A therapist may also teach you to apply athletic taping to support the bottom of your foot. Modalities include cold compression therapy, contrast bath therapy, iontophoresis and weight loss.
3. Orthotics.
- Your doctor may prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to your feet more evenly.
4. Night splints.
- Your doctor may recommend wearing a splint fitted to your calf and foot while you sleep. This holds the plantar fascia and Achilles tendon in a lengthened position overnight so that they can be stretched more effectively.
5. Oral Medications:
- To relieve pain and inflammation, nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen are often used but are of limited benefit. Patients should be encouraged to lessen activities which place more pressure on the balls of their feet because it increases tension in the plantar fascia.
6. Corticosteroid Injection at the site of pain.
- This modality often gives temporary or permanent relief, but may be painful, especially if not combined with a local anesthetic and injected slowly with a small-diameter needle. Repeated steroid injections may result in rupture of the plantar fascia.
7. Therapeutic ultrasound
- It has been shown in a controlled study to be ineffective as a treatment for plantar fasciitis. More recently, however, extracorporeal shockwave therapy (ESWT) has been used with some success in patients with symptoms lasting more than 6 months.
- Most patients ( over 95% ) should improve within one year of beginning non-surgical treatment, without any long-term problems. A few patients, however, will require surgery.
8. Surgery
- Surgical procedures, such as plantar fascia release, are a last resort, and often lead to further complications such as a lowering of the arch and pain in the supero-lateral side of the foot due to compression of the cuboid bone. The most common procedure is a partial plantar fasciotomy that may be either open or closed. An open procedure requires a 3-6 cm plantar medial incision to release the fascia. Nerve decompression and/or resection of calcaneal spur may also be performed at this time. A closed procedure utilizes endoscopy to release the fascia. An ultrasound guided needle fasciotomy can be used as a minimally invasive surgical intervention for Plantar Fasciitis. A needle is inserted into the Plantar Fascia and moved back and forwards to disrupt the fibrous tissue.
Alternative Medicine
- a. Magnetic Insoles
- Use of magnetic insoles has been considered by some clinicians as a treatment for PF, but available data regarding efficacy is limited, and results are mixed at best.
- b. Acupuncture
- Acupuncture has been proposed as an effective treatment for PF
- c. Nutritional Considerations
- -Vitamin C
- Widely known for its antioxidant properties, vitamin C is also an essential component for healthy connective tissue repair. A deficiency in vitamin C can result in abnormal collagen fibers, as well as other changes in the intracellular matrix, that can contribute to decreased tensile strength of fibrous tissues, such as those found in the plantar fascia. Recommended dosing of vitamin C for the purpose of tissue repair is 1-3 g daily until resolution.
- -Zinc
- Zinc, an essential trace mineral, is utilized in over 300 known enzymatic reactions. It is a key element in tissue regeneration and repair, working in concert with vitamin C to increase tensile strength of wounded tissue.
- Recommended dosage for zinc is 15-30 mg daily. (47,48)
- -Glucosamine
- Glucosamine may be helpful in the management of PF because it serves as a potential alternative to NSAID use and is a key biochemical component in the repair and regeneration of connective tissue. Glucosamine is the foundational structure of many compounds associated with repair and regeneration of connective tissue. It is the essential substrate for hyaluronic acid and other glycosaminoglycans used in maintaining healthy joint function. In vitro studies suggest glucosamine stimulates the synthesis of glycosaminoglycans and collagen. Recommended dosage for glucosamine is 500 mg three times daily in the form of glucosamine sulfate.
- -Bromelain
- Bromelain is the singular name used for a family of proteolytic enzymes found in the pineapple plant. Bromelain is commonly used in treating inflammation and soft tissue injuries and, as such, may be beneficial in the management of PF. It has been shown to accelerate healing from bruises and hematomas. It was reported that use of bromelain reduced swelling, tenderness, and pain, both at rest and during movement.
- There are several designations used to indicate the activity of bromelain. The most common measures of bromelain activity are milk clotting units (mcu) and gelatin dissolving units (gdu). One gdu approximately equals 1.5 mcu. Typically, enzymatic activity is given as a measure of mcu or gdu per gram of bromelain; e.g., 2,000 mcu/g or 1,333 gdu/g, respectively
- -Fish Oil
- These fish oils have been observed to suppress production of inflammatory mediators in patients with autoimmune conditions, such as rheumatoid arthritis. This may be due to reduced synthesis of key inflammatory mediators–leukotrienes, interleukin-2, and tumor necrosis factor. Such anti-inflammatory properties may in turn be beneficial in the management of PF. Recommended dosage for PF is 2-3 g daily.
Homeopathy
Homeopathy wise, consider the use of Bryonia 30C and Arnica 30C 4 pillules 3-4 times a day.

Leave a Reply